Lymphedema Care
Compression Bras After Breast Cancer:
What to Know
After breast cancer surgery or treatment, many people wonder what kind of bra will feel best, help with recovery, and possibly reduce swelling. The right compression bra can provide comfort, support, and confidence during a time when the body is adjusting and healing.
While not every woman needs compression, understanding the options available—and how to use them safely—can make a big difference.
Why a compression bra?
A well-fitted, supportive bra can reduce early post-operative pain and help you feel secure while tissues heal. Some women also use compression bras (or a standard, firm sports bra) to manage breast or chest wall swelling (breast or truncal lymphedema).
Evidence is growing but still mixed:
One randomized trial found a stable bra with compression reduced pain 3 weeks after surgery, while a pilot trial in women with breast edema after radiation found symptoms improved over time regardless of whether a compression-type sports bra or a standard bra was used (Johansson et al., 2020; OptiBra RCT, 2023; Verbelen et al., 2021).
What this means for you:
Supportive bras are reasonable early on for comfort; for breast-edema control, compression may help some people, but it isn’t universal—fit and comfort matter a lot, and your care team’s advice should lead (NCCN Survivorship Patient Guideline; ISL Consensus 2020).
Who typically benefits?:
-
Immediately after surgery (lumpectomy, mastectomy, reconstruction, or reduction): a soft, non-wired, front-closing, supportive bra—sometimes with light compression—can aid comfort and support for the first few weeks (Breast Cancer Now; OptiBra RCT).
-
Breast/chest wall (truncal) lymphedema: conservative care may include skin care, exercise, manual lymphatic drainage, and appropriately fitted compression bras/vests or targeted pads under the bra. Evidence is limited and individualized fitting is key (Verbelen et al., 2021; Cornacchia et al., 2022).
What features to look for (coverage & design):
-
Front closure (zip or hooks) for easy on/off and post-op shoulder comfort.
-
Wire-free cups and soft seams to reduce skin irritation; wide, adjustable straps to spread load.
-
High side panels and higher underarm/axilla coverage if you have underarm or lateral breast swelling.
-
Extended length/“vest” styles for chest wall/back involvement.
-
Pockets for breast forms and/or swell pads to target fibrosis or focal edema.
Note: Unlike arm sleeves, bras rarely list mmHg pressure; manufacturers label compression as “light/medium/firm.” Prioritize comfort and symptom response over a specific “number.”
Sizing & fit (how to get it right):
-
Expect shape/size changes for up to a year after surgery or radiation—re-measure periodically.
-
Measure underbust and full bust; if using S–XXL sizing, follow each brand’s chart and consider trying two adjacent sizes.
-
If possible, get fitted by a certified mastectomy/lymphedema fitter—they can also advise on pads and strap adjustments.
When and how long to wear it
-
Immediately after surgery: many teams recommend wearing a supportive (often lightly compressive) bra day and night for the first 2–6 weeks, removing only to bathe, then taper based on comfort and surgeon guidance.
-
For breast/chest lymphedema: wear during the day and during activities that worsen swelling; adjust daily hours to comfort and response. In a pilot study after radiation, women wore the assigned bra daytime for 9 months.
How to wear (practical steps)
-
Start on the loosest setting (or unzip), place pads if prescribed, then close from the front.
-
Check the edges: the band and side panels should be snug but not biting; no “rope-like” lines.
-
Do a breath & arm check: you should breathe comfortably and move your arms without pinching.
-
Re-check fit later in the day—swelling can fluctuate.
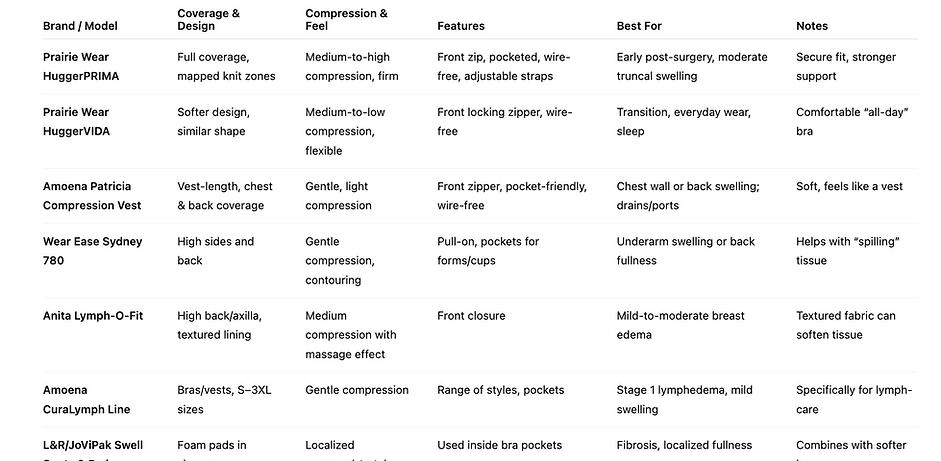
Popular examples & how they differ:
Prairie Wear HuggerPRIMA
-
Full coverage with mapped knit zones for structured compression.
-
Firmest in the Prairie Wear line, providing medium-to-high compression.
-
Front zip closure, wire-free, with pockets and adjustable straps.
-
Ideal for the early post-surgery period or moderate truncal swelling.
-
Patients often find it the most secure, though less “soft” than others.
Prairie Wear HuggerVIDA
-
Softer, more flexible design, with medium-to-low compression.
-
Features a front locking zipper and wire-free support.
-
Popular for everyday comfort, transition from firmer compression, or even sleeping.
-
Many describe it as the easiest to wear “all day long.”
Amoena Patricia Compression Vest
-
Vest-length design gives gentle, uniform compression across chest and back.
-
Soft and non-restrictive, with a front zipper and pockets for forms or pads.
-
Useful for women with chest wall/back swelling, or those with drains/ports.
-
Often chosen for its extended coverage without feeling too tight.
Wear Ease Sydney 780
-
High side and back panels provide contouring and gentle compression.
-
Pull-on style with pockets for cups or forms.
-
Designed to help underarm swelling or back tissue fullness, especially if tissue “spills” to the sides.
-
Comfortable for daily activities while controlling shape and swelling.
Anita Lymph-O-Fit
-
Features a unique textured inner lining intended to stimulate lymphatic flow.
-
Provides medium compression with a “massage-like” feel.
-
Front closure for ease of use.
-
Best for women with mild-to-moderate edema or firm tissue that benefits from texture.
-
Takes some adjustment as the texture feels different at first.
Amoena CuraLymph Line
-
Specifically designed for women with lymphedema or at risk of it.
-
Gentle compression, with bras and vests available in S–3XL.
-
All styles come pocketed for forms or pads.
-
A good starting point for mild swelling or stage 1 lymphedema.
-
Combines comfort with medical-grade support.
L&R/JoViPak Swell Spots & Pads
-
Foam-filled pads in various shapes (breast swell spot, lateral breast pad, inframammary fold pad).
-
Used inside the pocket of almost any bra.
-
Provide localized pressure to soften fibrosis or target areas of swelling.
-
Very versatile, often paired with softer bras for tailored therapy.
Precautions & contraindications:
-
Avoid or pause compression over open wounds, severe skin reactions, or infection.
-
Cardiac concerns: decompensated heart failure or pulmonary edema are contraindications; stable cases require medical oversight.
-
Arterial disease: severe peripheral arterial disease is a contraindication for strong compression.
-
Comfort matters: if the bra feels too tight, restricts breathing, or causes numbness, it should be adjusted or replaced.
A simple “start-here” plan:
-
Ask your care team which style to begin with.
-
Try two sizes of a front-closing, wire-free, high-side bra; add pads only if recommended.
-
Wear day & night for the first weeks post-op (if advised), then taper; for lymphedema, use during the day and when more active.
-
Reassess monthly—as swelling and healing change, your “best” bra may change too.
Scientific References:
-
Cornacchia, C., et al. (2022). Breast edema after conservative surgery for early-stage breast cancer. Lymphology.
-
Executive Committee of the International Society of Lymphology. (2020). The diagnosis and treatment of peripheral lymphedema: 2020 consensus document. Lymphology, 53(1), 3–19.
-
Johansson, K., et al. (2020). Compression treatment of breast edema: A randomized controlled pilot study. Lymphatic Research and Biology.
-
Morgan, R. L., et al. (2020). ONS Guidelines™ for cancer treatment–related lymphedema. Oncology Nursing Society.
-
NCCN. (2024). Survivorship: Patient Guidelines.
-
OptiBra Study Group. (2023). Optimal bra after breast cancer surgery—stable bra with compression reduces early pain. The Breast.
-
Rabe, E., et al. (2020). Risks and contraindications of medical compression treatment. Phlebology/Lymphology.
-
Saini, R., et al. (2024). Brassiere-wearing practices and issues among post-surgical breast cancer survivors: Systematic review. Patient Preference and Adherence.
-
Verbelen, H., et al. (2021). Breast edema after breast-conserving therapy: State of the art. Archives of Physiotherapy.
-
Breast Cancer Now. (n.d.). Bras after surgery for breast cancer.